The Top 7 Things to Avoid with Degenerative Disc Disease for a Pain-Free Life
From poor posture to eating certain foods, learn the top seven things to avoid with degenerative disc disease for prevention and to maintain a healthy spine.
Knowing what things to avoid with degenerative disc disease may be tricky. Patients with degenerative discs receive recommendations to exercise, but they shouldn’t exercise too hard. They should avoid certain foods, but not others. Maintaining a healthy posture is important, but what does that even mean? To dispel some of the confusion, we compiled a list of what to avoid if you have degenerative disc disease and helpful practices to adopt instead.
Disc degeneration impacts roughly 27.3 percent of Americans to some degree. While some patients with degenerative disc disease are asymptomatic, others develop severe, persistent back or neck pain. Fortunately, there are actionable, effective ways to live a pain-free life, no matter the severity of disc degeneration.
Understanding Degenerative Disc Disease
Spinal discs allow our backs to bend and twist. Whenever you do an upward dog in a yoga class or lift heavy boxes, your spinal discs are to thank. As we age, some wear and tear on spinal discs is normal. Disc degeneration can cause problems when it interferes with everyday tasks.
“If you’re an avid tennis player, you deserve to be able to play tennis without your back preventing you. If you can’t, that would be considered degenerative disc disease,” explains Neil Bhamb, MD, an orthopedic spine surgeon and the medical director of concierge care at Commons Clinic.
He adds that degenerative disc disease is more than just a minor bother; it stops you from doing activities you enjoy and day-to-day tasks, such as playing with your kids or cooking pain-free. If the pain has not reached that level, it wouldn’t necessarily be considered disease level.
What is Degenerative Disc Disease?
The word “disease” is deceiving. Degenerative disc disease isn’t a disease but a condition where discs in the back, typically in the cervical or lumbar region, break down. This deterioration may cause pain ranging from moderate to severe. Pain is often experienced in the neck, butt, thighs, and arms. It may come and go or be persistent, and it is usually worse when twisting your back or neck, picking up something heavy, or when seated.
The pain caused by degenerating discs can limit your range of motion and the ability to lift heavy objects. Degenerative discs may also make you more susceptible to injury due to impact or stress in the back. If left untreated, degenerative discs can also cause nerve and spinal damage.
Causes and Stages of Degenerative Disc Disease
“Degenerative disc disease is really a mix of lots of different disorders,” says Dr. Bhamb. “A good third of it is due to what you do, probably about a third is due to your genetics, and perhaps a third is random luck.”
Degenerative disc disease can be connected to osteoarthritis, a condition that can wear down discs in the back, but tears from sports or everyday life can cause it as well. Various collagen-producing genes and proteins have been associated with a higher risk of degenerative disc disease, though researchers are still uncertain why this connection exists.
Pain is often the first sign of a degenerative disc. Simply feeling pain can be thought of as the first “stage” of the condition. At this point, it’s best to create an appointment with a primary care doctor who can refer you to the right specialist. This may include a spine specialist or surgeon, who performs neck and back surgery. If your condition does not require surgery, you may be referred to a pain management specialist, who can create a treatment plan that may include physical therapy and lifestyle changes.
If the discs continue to degenerate, they can move and press against spinal nerves. When this happens, you may feel weakness or numbness in the nerves. At this stage, a pain management specialist will design a more robust treatment plan that may include pain medications, back surgery, or more intensive physical therapy.
Sometimes, disc degeneration also triggers outgrowths, bone spurs that form along the spine and pinch or compress the spinal nerve. If this kind of spinal damage progresses, more serious symptoms may develop, such as:
- Trouble walking
- Problems with bladder control
- Difficulty controlling bowel movements
- Nerve damage
- Weak or numb arms and legs
Avoiding Physical Strains
Physical strains are the most important thing to avoid to prevent disc degeneration. Physical strains can trigger disc degeneration, causing sudden or gradual pain. Strains can also cause a disc to “out-pouch” and press against the spinal nerve, creating potential for nerve or spine damage.
Avoiding physical strains sounds easy in theory, but may be more difficult in practice because it requires you to rethink how you lift heavy loads. When lifting anything, it’s best to practice proper lifting techniques, but it’s especially important when dealing with heavy loads, such as a weight at the gym or a box of seasonal decor at home.
Stanford University outlined some of the best lifting techniques:
- Use equipment, like a cart, to hull heavy loads when available
- Assess how heavy something is before lifting. When it weighs too much, ask a friend or colleague for help.
- Disassemble larger objects into smaller, lighter ones, when possible
- Take frequent breaks and use those breaks to stretch
Avoid Overexercising
While exercise is recommended for those with degenerative disc disease, the gym is also a prime spot for accidental strains due to improper form, increasing your intensity too fast, or overuse.
To avoid injury, be careful with your workouts, and remember these tips:
- Don’t be a “weekend warrior”: Combining all your workouts into a few intense sessions sounds like a great way to save time, but it isn’t helping your back. The United States Department of Health and Human Services (HHS) recommends moderate aerobic exercise, like brisk walking, swimming, or biking, on a daily basis. What is considered moderate may differ based on fitness level and pain experienced, making it important to build an appropriate workout routine with a physical trainer or other medical expert.
- Stretch gently: Add gentle stretching to your routine, especially when disc pain flares up. Bryan Wright, DPT, a physical therapist and owner of Wright Physical Therapy in Twin Falls, Idaho recommends child’s pose, cat/cow pose, and bridge pose for those with degenerative disc disease. To determine the best stretches for you and the ideal time length for a session, consult a physician or physical therapist.
- Avoid heavy lifting: Weightlifting places pressure on the spine and discs around the spine. To avoid disc degeneration, don’t switch weight classes too quickly as this may increase the chance of injury. When possible, opt for machines over free weights since machines place less weight on the spine and don’t require a spotter.
- Do ab workouts: Exercises for the ab and core muscles can sometimes help speed up back pain recovery and avoid future flare-ups. When you do ab exercises, such as planks or crunches, you strengthen the abdominal muscles, taking some stress off the spine. However, it’s best to follow a doctor or physical therapist’s guidance on ab workouts since they are not usually recommended when experiencing back pain.
- Don’t run improperly: Running can jar and compress the discs in the lower back, especially when your shoes don’t have enough cushion or your running posture is off. If running, pay attention to shoes and posture. Shoe stores specializing in running shoes are good resources for finding the right shoe for your exercise needs. And remember to stretch before and after your run.
Maintaining a Healthy Posture
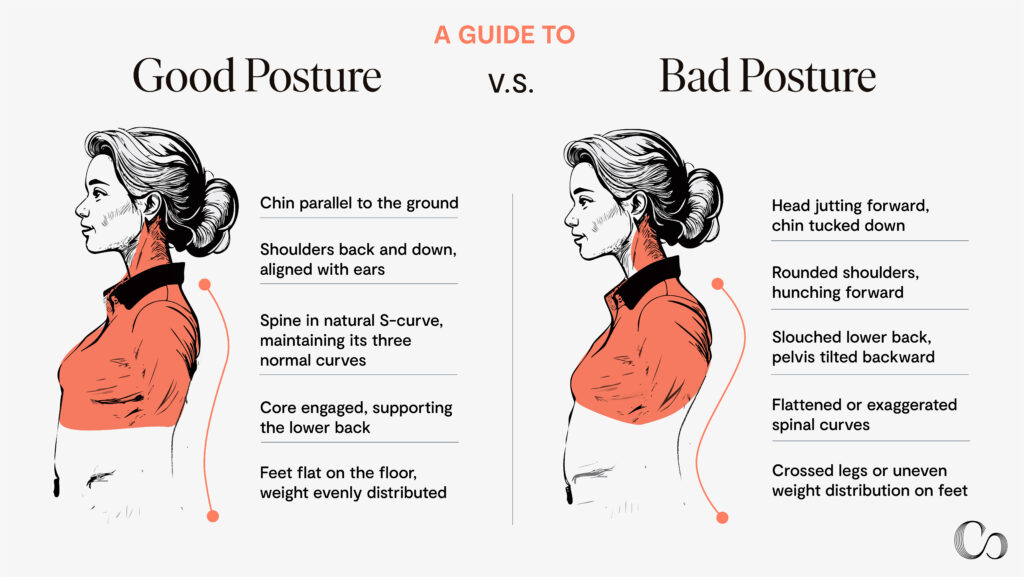
Your posture may slip during a long day at work or during a Stranger Things marathon—and that can cause disc degeneration. A 2021 study in the journal Open Medicine found poor posture increases the risk of disc degeneration. More specifically, this study analyzed the relationship between posture and degenerative disc disease in 113 patients. Researchers found those who spend significant time with their spine curved forward were at higher risk for disk degeneration.
The challenge is that what constitutes good posture differs from person to person, says Dr. Bhamb. There is, however, one general rule we can all follow. Dr. Bhamb explains, “Imagine that your spine is attached with a little string in your head and try to stand as tall as possible, as if you can pull that string. That will help you to sort of assume the best posture for you, no matter who you are.”
Another general posture rule? Avoid sitting for long periods of time. A small 2020 study published in the European Journal of Pain analyzed lifestyle choices and the risk for different types of back pain. They found participants who moved less throughout the day were at greater risk for almost all types of back pain.
If you work a desk job, consider adding in small stretch breaks every few hours or moving your body during your lunch break or after work.
Dietary Considerations for Degenerative Disc Disease
While not as obvious, your diet also plays a role in reducing disc degeneration and pain. One 2023 study linked inflammatory foods, like baked goods and processed meat, to a 40 percent higher risk of joint pain and stiffness. While the study did not discover causation between diets high in inflammatory foods and back pain, it did find a correlation.
Plus, an inflammatory diet has been linked to a higher body mass index (BMI), a measure of your height against your weight. When someone’s BMI is in the overweight or obese category, that weight increases pressure on the back, potentially causing discs to wear down.
To adopt an anti-inflammatory diet, consider these swaps:
- Swap processed snacks for nuts, seeds or fruit
- Trade processed red meats for unprocessed cuts or alternatives, like fish
- Switch processed carbs, like white bread, for whole grains, like quinoa
- Adapt elements of diets that are naturally anti-inflammatory, such as the Mediterranean or Japanese diet
Managing Degenerative Disc Disease
One thing you shouldn’t avoid if you have degenerative discs? The physical therapist. In fact, pain from disc degeneration can improve in as little as six weeks of physical therapy. Typically, physical therapy for disc degeneration will focus on stretches and ways to strengthen the core and relieve back pain. Since pain often gets worse with a sedentary lifestyle, a physical therapist can also help you adapt your lifestyle to be more active (safely).
Physical therapy is typically covered by insurance, though you may have to pay a copay per visit. The exact copay amount depends on your insurance plan. Sometimes, sessions can even be free up to a certain number or after the plan’s deductible is reached.
Orthopedic surgeons and pain management specialists are often the referring doctors. At Commons Clinic, for example, our surgeons refer patients to in-house physical therapists. The referred PT will assess your condition and current lifestyle and develop a plan that may involve reducing back pain, improving posture, and instructing on form for exercises.
Whether as a standalone treatment or in tandem with other treatments, Dr. Bhamb recommends physical therapy focused on mobility and living a more active lifestyle.
Ergonomic Adjustments for Daily Life
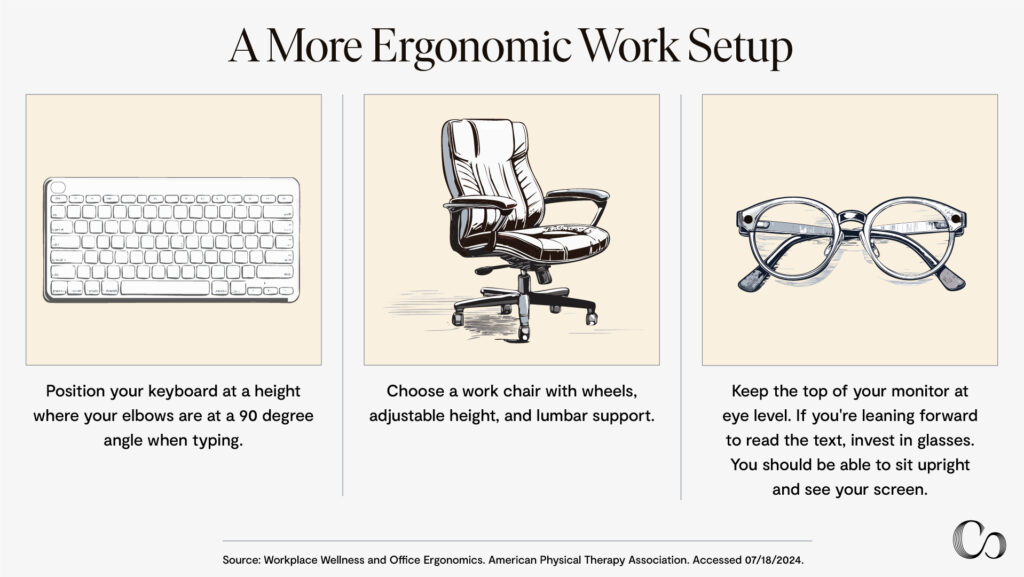
A large portion of our days are spent at work or in the car. According to U.S. Census data, Americans commute about 52 minutes to and from work daily and spend 7.75 hours a day working on average.
However, our cars and desks are seldom designed to be ergonomic, or ideal to minimize pain and improve posture. Fortunately, there are some easy fixes.
The American Physical Therapy Association outlines three key changes for a more ergonomic work setup:
- Choose a work chair with wheels, adjustable height and lumbar support.
- Position your keyboard at a height where your elbows are at a 90 degree angle when typing.
- Keep the top of your monitor at eye level. If you find yourself leaning forward to see the text, invest in glasses since you should be able to sit upright and see your screen.
When it comes to an ergonomic car ride, posture matters more than anything else. One 2022 study with 384 participants found a strong correlation between lower back pain and those who drove with poor posture.
According to the study, driving with bad posture increased the chance of degenerative disc disease by 51 percent. The researchers added the correct driving posture is to sit with your back straight against the car seat and legs uncrossed and extended on the floor in front of you.
Avoiding Overmedication and Surgery
Surgery and medication can be successful at treating pain from degenerative disc disease. However, both options also have serious side effects and out-of-pocket costs. While medication can work in moderation and surgery is a great first resort, they aren’t the last resort for treating or preventing degenerative disc disease.
Risks of overusing medications for degenerative disc disease
According to the HHS, medication is often the first step in treating back pain. Analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), opioids, and anticonvulsants are commonly prescribed for persistent back pain.
While these medications can be effective, depending on the prescription and pain severity, using them for long periods of time or in large doses can cause side effects such as drowsiness, nausea, itching, and addiction and withdrawal. NSAIDs can cause stomach ulcers or damage to the liver and kidneys if taken regularly. A 2022 meta-analysis found reliance on medication to treat back pain didn’t create sustainable change. Instead, the researchers suggest treatment plans with lifestyle changes and exercises, often accompanied by some medication, resulted in less pain long-term.
When to avoid surgery for spinal disc problems
“The best time to see a surgeon is when you’ve tried some other things, and they didn’t work,” says Dr. Bhamb. A lot of the patients he sees are in their 40s, live an active lifestyle, and have dealt with degenerative discs for five to 10 years. If physical therapy and medications aren’t working, Dr. Bhamb says they may be a good candidate for surgery.
When surgery is required, degenerate discs are usually replaced, protecting the other discs. “Now that we’ve been through several generations of the surgery, the outcomes are quite promising,” says Dr. Bhamb. He notes after recovery that many of his patients can resume exercise and hobbies with less pain than before surgery.
Surgery, however, can be a significant expense, depending on healthcare coverage, and it requires time off work. Dr. Bhamb recommends seeing it as an investment—and one that will require additional physical therapy and possible lifestyle changes after.
Consider surgery when conservative treatments have failed to provide relief over an extended period, typically 6-12 months. If you’re experiencing persistent pain that significantly impacts your quality of life, interferes with daily activities, or causes neurological symptoms like weakness or numbness, it may be time to consult a surgeon. Additionally, if diagnostic imaging shows severe disc degeneration or compression of nerves, surgery might be recommended sooner. Always discuss the potential benefits and risks with your healthcare provider to determine if surgery is the right option for your specific condition and circumstances.

Frequently Asked Questions (FAQs)
How effective are treatments like chiropractic care or acupuncture for DDD?
Chiropractic care and acupuncture can be effective at treating low back pain associated with degenerative disc disease. Thanks to its efficacy, the Center for Medicare and Medicaid recently approved 90 days of acupuncture for low back pain, and other insurance companies may do the same. However, not all insurance companies cover these practices, and more research is required to confirm their effectiveness. A more established alternative, often covered by insurance when prescribed by a doctor, is physical therapy.
Can weight loss help reduce the symptoms of degenerative disc disease?
Weight loss is a great lifestyle intervention to reduce the symptoms of degenerative disc disease. This condition is often caused by “wear” or stress on the discs, which can be caused by excess weight or inflammation.
Can degenerative disc disease lead to other complications or conditions?
Degenerative disc disease is marked by back pain and difficulty doing everyday tasks, such as picking up something heavy or twisting the spine. If the condition progresses, it can lead to spine or nerve damage, which can cause pain and disruption throughout the body, not just in the back.
What is the prognosis for someone with degenerative disc disease?
Degenerative disc disease is not life-threatening and with the right treatment, current pain can be minimized and future pain prevented. However, the most effective treatment is often a combination of physical therapy or pain medication and lifestyle changes, including improving posture, exercising regularly, and eating an anti-inflammatory diet.
Are there any new treatments or research developments for degenerative disc disease?
Recent research emphasizes the role of lifestyle interventions in treating degenerative disc disease. These developments stem from more people sitting at work, which can cause poor posture and back pain, and from recent research emphasizing diet and exercise’s role in preventing degenerative disc disease.
Can degenerative disc disease lead to disability or require long-term care?
Since degenerative disc disease can cause chronic pain and spine or nerve damage, it can lead to disability and a need for long-term care. However, this is only in severe cases. With the right treatment plan, it doesn’t have to impact your day-to-day life.
How often should I follow up with my doctor to monitor the progression of my condition?
Your doctor will recommend a specific follow-up time based on the severity of the degenerative disc disease. If physical therapy is recommended, weekly or biweekly appointments may be established.
Conclusion
“Disc degeneration is super treatable,” says Dr. Bhamb, “But it’s not just about treatment. It’s about changing a lifestyle.” Committing to an active lifestyle coupled with a healthy diet, regular exercise and creating an ergonomic work space can help manage degenerative discs and prevent future symptoms.
If pain persists after making lifestyle changes or if confused on what changes are right for you, contact a physician for a consultation. Together, you can create a rehabilitation plan to get you back to your normal life.
Sources
Parenteau, Chantal S et al. “Prevalence of spine degeneration diagnosis by type, age, gender, and obesity using Medicare data.” Scientific Reports 11(1): 5389. 8 Mar. 2021. doi:10.1038/s41598-021-84724-6
Low Back Pain Fact Sheet. U.S. Department of Health and Human Services. Accessed 07/18/2024.
Arthritis Foundation. Degenerative Disc Disease. Accessed 07/18/2024.
Back Pain. National Institute of Arthritis and Musculoskeletal and Skin Diseases. Accessed 07/18/2024.
Donnally Chester et al. Lumbar Degenerative Disk Disease. Accessed 07/18/2024.
Intervertebral disc disease. National Library of Medicine. Accessed 07/18/2024.
Safe Lifting. Stanford Environmental Health and Safety.
Back Pain and Sports. National Library of Medicine. Accessed 07/18/2024.
Lee, Hyo Jeong, et al. “Correlation between kinematic sagittal parameters of the cervical lordosis or head posture and disc degeneration in patients with posterior neck pain.” Open Medicine 16(1): 161-168. 2021. https://doi.org/10.1515/med-2021-0219
Wernli Kevin et al. “Movement, posture and low back pain. How do they relate? A replicated single-case design in 12 people with persistent, disabling low back pain.” European Journal of Pain. 04 July 2020. https://doi.org/10.1002/ejp.1631
Khamoushi Firoozeh et al. “Association between dietary inflammatory index and musculoskeletal disorders in adults.” Scientific Reports 13: 20302. 13 Nov 2023. doi:10.1038/s41598-023-46429-w
de Mello, Roseli Neves et al. “Dietary inflammatory index and its relation to the pathophysiological aspects of obesity: a narrative review.” Archives of Endocrinology and Metabolism 67(6): e000631. 2023. doi:10.20945/2359-3997000000631
Getting started on the Mediterranean diet. Ohio State University. Accessed 07/18/2024.
Wang, Yu et al. “The Effects of Red Meat Intake on Inflammation Biomarkers in Humans: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Current Developments in Nutrition 6(1). 14 June 2022, doi:10.1093/cdn/nzac068.023
Herniated disk. National Library of Medicine. Accessed 07/18/2024.
United States Commuting At A Glance: American Community Survey 1-Year Estimates. U.S. Census Bureau. Accessed 07/18/2024.
American Time Use Survey. Bureau of Labor Statistics. Accessed 07/18/2024.
Workplace Wellness and Office Ergonomics. American Physical Therapy Association. Accessed 07/18/2024.
Atallah, Ayman A et al. “Prevalence of Lower Back Pain and its Relationship with Driving Postures among Drivers in Taif, Saudi Arabia.” Journal of Pharmacy & Bioallied Sciences 14. 2022. doi:10.4103/jpbs.jpbs_882_21
Medicines for Back Pain. National Library of Medicine. Accessed 08/06/2024.
Kühn, L., et al. “Research designs and instruments to detect physiotherapy overuse of low-value care services in low back pain management: a scoping review protocol.” Systematic Review 11(212).2022. https://doi.org/10.1186/s13643-022-02083-3
Evaniew N, et al. “Lumbar Fusion Surgery for Patients With Back Pain and Degenerative Disc Disease: An Observational Study From the Canadian Spine Outcomes and Research Network.” Global Spine Journal 12(8):1676-1686. 2022. doi:10.1177/2192568220985470





 (310) 574-0414
(310) 574-0414