Signs a Herniated Disc Is Healing: The Ultimate Guide to Recovery
A herniated disc can disrupt your life, but healing is possible. Learn how to recognize the key signs of recovery and what to expect as you heal.
With the passage of time, your body begins to grumble and groan in ways you never expected. Joints that once moved effortlessly now stiffen and resist, while muscles tighten like overworked rubber bands. Your tendons and ligaments lose their springy resilience, turning quick recoveries into lengthy ordeals. Before you know it, one restless night can leave you feeling like a statue, your neck and back stubbornly refusing to budge.
Nearly 80 percent of people will experience lower back pain at some point in their lives. 1 Aging, trauma, and repetitive motions that affect your spine and back can cause lower back pain. For some, this lower back pain may be caused by a herniated disc.
However, back pain is not a reason to immediately panic or worry. If you have been diagnosed with a herniated disc or think you may have one, this article will help you know what to expect, recognize the signs your herniated disc is healing, and learn how to thrive after healing.
What is a herniated disc?
A herniated disc occurs when a fragment of a spinal disc is forced through a weakened part of the spine and into the spinal canal. The weakened spine is common with aging, making the disc more likely to tear or rupture. A herniated disc is often referred to as a slipped, bulged, or ruptured disc. The injury can occur in any part of the spine, but usually occurs in the lower back and the neck. This is because the lower back and neck are flexible, experiencing frequent stress from twisting, pulling, and lifting objects.
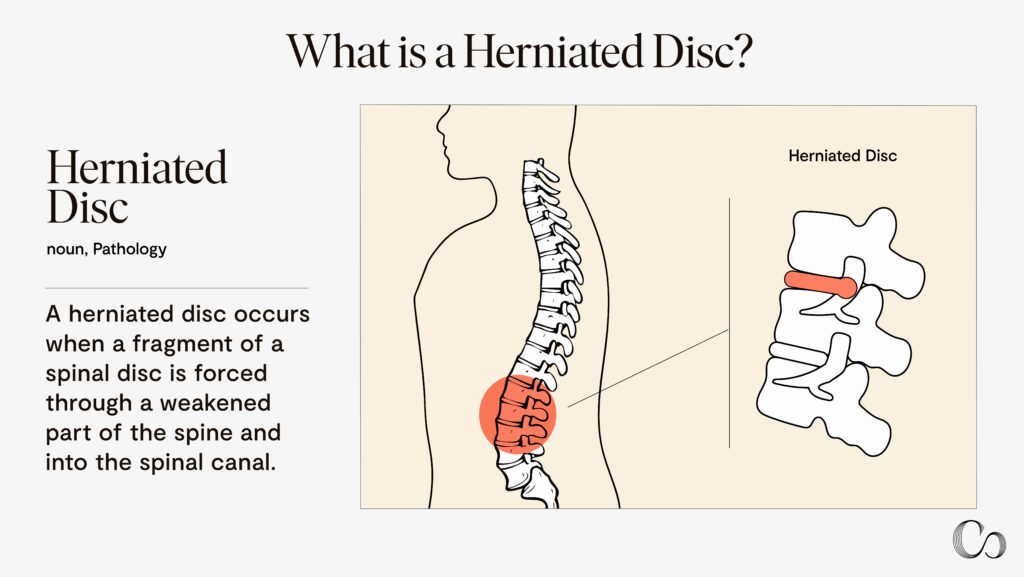
Depending on where the herniated disc occurs, it may cause pain, numbness, or weakness in the arm or leg. The herniated disc can also irritate or compress nearby nerves, pinching them and causing pain, numbness, tingling, or weakness.
Most people cannot pinpoint exactly what caused their herniated disc. However, the most common cause of a herniated disc is gradual aging and wear over time. The spinal discs become less flexible as you age and are more prone to tearing or rupturing. It is possible to tear or rupture a disc if you lift with your back instead of your legs or if you twist while lifting. However, it is very rare that a fall or blow to the back will cause a herniated disc.
Symptoms of herniated discs
Symptoms related to a herniated disc depend on where the herniation occurs. It is possible to have no symptoms with a herniated disc. However, some common symptoms of a herniated disc include:
- Lower back disc: pain in lower back, buttocks, thigh, calf, or foot
- Neck disc: pain in the shoulder or arm
- Sharp, burning pain when coughing or moving
- Numbness, tingling, and difficulty lifting objects
- Muscle spasms from pinched nerves
- Mood changes, depression, and anxiety from pain
- Difficulty standing or walking
- Loss of bladder control from nerve compression
It’s important to understand that these symptoms arise from a disruption to the spine’s natural function. As Neil Bhamb, M.D., a Commons Clinic spine surgeon and director of concierge services, notes, “The core of the spine is designed to move. When we’re born, we use our spines, and we use the movement of our spines to do almost everything. Even sitting in a chair versus lying down in a bed or standing up or actually moving, our spine might feel like it’s pretty straight, but we’re actually moving the whole time.” A herniated disc interferes with this constant, subtle movement, leading to various symptoms and complications.
Living with a herniated disc can also negatively affect your mood, increasing feelings of depression and anxiety, particularly due to chronic pain and loss of sleep. Depending on the location and severity of the herniated disc, you may have difficulty standing or walking, with a lumbar herniated disc causing worsened pain when standing, walking or sitting. In severe cases, nerve compression from the herniated disc can lead to loss of bladder control, resulting in incontinence.
Risks of developing a herniated disc
Your risk of developing a herniated disc increases if you have excess body weight, which can cause additional stress on the discs in the lower back. Some people are also predisposed to developing a herniated disc because of genetics due to lumbar disc herniation clusters.
Studies show that around 75 percent of degenerative disc disease is hereditary.5 The aggrecan (AGC1) gene can increase the risk of disc bulge and intervertebral disc disease. The collagen IX gene has been linked to lumbar disc herniation and sciatica. The SKT(KIAA1217) gene has been associated with lumbar disc herniation. Generally, if you have relatives with degenerative disc disease, it is important that you focus on modifying your risk factors.
The type of work you do can also increase your risk for developing a herniated disc. Some professions most at risk include construction workers, factory workers, nurses, landscapers, and mechanics. If your job is physically demanding and requires repetitive lifting, pulling, pushing, bending sideways, and twisting, this can increase your chance of developing a herniated disc.
If you drive for work, you may be at an increased risk of developing a herniated disc. In these jobs, sitting for long periods combined with the vibration from a motor vehicle engine can put pressure on the spine, eventually leading to a herniated disc. Smoking also increases your risk profile for having a herniated disc. Studies show smoking lessens the oxygen supply to the spinal discs, causing them to break down more quickly and lead to a herniated disc.2
The Herniated Disc Healing Process
A herniated disc heals over time and will differ with each person. “There are some definite factors that influence the rate of healing, but it is still impossible to predict,” says Georgiy Brusovanik, MD, orthopedist/spine and bone specialist at Miami Spine Doctor.
During the acute inflammation stage, the inflammatory response is at its peak. Individuals who are younger, especially kids, have more inflammation compared to an elderly person.
“Elderly individuals should be able to get better faster since their inflammation will die down,” he says. “On the other hand, a strong, inflammatory response, like with younger persons, helps clear the herniated disc and may make improvement come faster.”
There are multiple reasons why this may occur. For one, the inflammatory response causes the herniated material to shrink and the inflammatory proteins near the root nerve to decrease. The body may also release enzymes to clear away the herniation.
The size of the herniation matters as well as the location. Large herniation has a higher chance of compressing and hurting a nerve than a small herniation. If a herniation is located close to the midline, where there is more area for the nerves, that herniation may cause less pain.
“If a herniation is closer to the edges of the canal where the nerves cannot get away, there is a higher chance that [the patient] will be symptomatic,” explains Dr. Brusovanik. The spinal canal, also called the vertebral canal, is a space filled with fluid in the spinal column that protects the spinal cord and nerve roots.
The underlying health of the disc makes a difference as well. If a disc is more degenerative, the patient may continue to suffer, even after the herniation itself has resorbed. Resorption of the herniated disc, or spontaneous shrinkage, happens when the jelly-like material inside the spinal disc squeezes out and is exposed to other tissues. The tissues create chemicals that break down the material, which is gradually absorbed by the body.
The good news is that the vast majority of disc herniation gets better without surgery. “Unless you are experiencing significant numbness or weakness in the extremities, it is reasonable to keep trying to get better with conservative/non-surgical means,” advises Dr. Brusovanik.
Signs of Healing
Reduced Pain and Discomfort
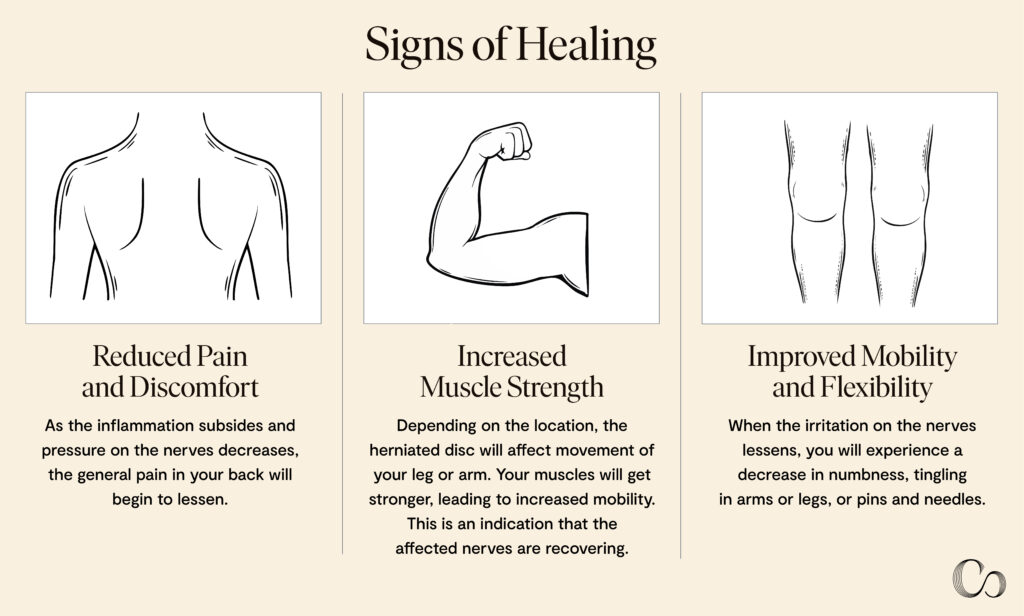
“The signs of healing are pretty well defined. The pain disappears first, then numbness is usually the second to go, and if there [was] some weakness, it is the last to get better,” says Dr. Brusovanik.
As the inflammation subsides and pressure on nerves decreases, the general pain in your back will begin to lessen. If you have sciatica or leg pain, a reduction in its intensity or spread down the leg is a sign that you’re healing. As your pain decreases, you’ll be able to move more freely without discomfort. Being able to move or bend without severe pain is a sign of healing.
Improved Mobility and Flexibility
Another sign of healing is a return to normal sensation. When the irritation on the nerves lessens, you will experience a decrease in numbness, tingling in arms or legs, or pins and needles. As you heal, the muscle spasms around the affected area should relax and decrease. This will allow you to move more freely and have greater flexibility.
Increased Muscle Strength
Herniated discs may cause weakness along the path of the affected nerve because the nerve is unable to function correctly. Depending on the location, the herniated disc will affect movement of your leg or arm. As the healing process progresses, your muscles will get stronger, manifesting in increased mobility. This is an indication that the affected nerves are recovering.
Treatment and Rehabilitation Options
In most cases, a physical exam and review of your medical history are the only things needed to diagnose a herniated disc. For others, a herniated disc is diagnosed after a physical exam, imaging tests, and nerve tests. The physical exam includes a neurological exam to check your reflexes, muscle strength, walking ability, and your ability to feel light touches, pinpricks, or vibration.
Your doctor may order other tests like imaging if other complications exist. Imaging tests may include x-rays, CT scans, an MRI, or myelogram. An x-ray will not detect a herniated disc, but it will rule out other causes of back pain like an infection, tumor, spinal alignment issues, or a broken bone. An MRI will confirm the location of the herniated disc and which nerves are affected. A myelogram, more commonly known as a CT scan with contrast, can show pressure on the spinal cord or nerves due to multiple herniated discs or other conditions.
Nerve tests can help pinpoint the location of nerve damage using nerve conduction studies and electromyograms (EMGs) that measure how well electrical impulses are moving along nerve tissue.
Medications for Herniated Discs
Treatment for a herniated disc usually starts with a conservative approach, which includes changing and restricting movement that causes pain. Your healthcare provider may couple this with over-the-counter pain medications like acetaminophen (Tylenol), ibuprofen (Advil, Motrin IB), or naproxen sodium (Aleve).
Other options for pain medication are neuropathic drugs that affect nerve impulses to decrease pain. Some examples of these include gabapentin (Horizant, Neurontin), pregabalin (Lyrica), duloxetine (Cymbalta), or venlafaxine (Effexor XR). If you have muscle spasms, you may be prescribed muscle relaxers. Common side effects of muscle relaxers are sleepiness and dizziness. Your physician will determine a treatment plan that best suits you.
If other medications don’t relieve your pain, your healthcare provider may recommend short-term use of opioids like codeine or an oxycodone-acetaminophen combination (Percocet). The general guideline is to take the opioids for no more than five days. If none of these work, your physician may recommend cortisone injections, which are injected into the area around the spinal nerves.
Chiropractic Treatment for Herniated Discs
Chiropractors use spinal manipulation to help heal and may be a viable option for treating a herniated disc. Flexion-distraction technique is one such chiropractic option. With this technique, the patient lies on a table to stretch out the back and spinal column. The goal is to stimulate the disc while it is in a stretched-out position, since this allows the disc to be moved back into its correct place. This technique reduces pain because it helps move the disc away from the nerves.
Pelvic blocking techniques are another chiropractic treatment for herniated discs . For this treatment, the patient lies with cushioned wedges underneath the pelvic area. This position relieves pressure on the discs in the spine. Stretching out the lower pelvic area helps relieve any spinal pressure.
Another option is manipulating the spinal area while using anesthesia. This is recommended when a patient is experiencing a great deal of pain. This procedure takes anywhere from 15 minutes to one hour, and often requires being treated multiple days in a row. Depending on your level of pain, the chiropractor may choose to use a local anesthetic, mild sedation, or even general anesthesia.
Physical therapy
Physical therapy may be used as a complement to pain medication. A physical therapist will teach exercises that minimize pain caused by a herniated disc. Back extension exercises, in particular, have been shown to help herniated discs. Manual therapy techniques that include joint mobilizations to the lumbar spine, thoracic spine, and hip are also helpful. Your physician may recommend a physical therapist. Therapy may last anywhere between two to eight weeks (or even longer) depending on severity of the herniated disc, where it is located, your age, and overall health.
Surgical interventions
If these conservative approaches do not improve your symptoms after six weeks, you may need surgery. Surgery is recommended if you continue to have poorly controlled pain, numbness or weakness, trouble standing or walking, and loss of bladder or bowel control. Your physician will let you know when you need surgery.
During surgery, known as discectomy, the surgeon will remove the protruding portion of the disc. In rare cases when the entire disc must be removed, the vertebrae might need to be fused with a bone graft. Metal hardware is placed in the spine to provide spinal ability. This process allows for bone fusion, which takes months to complete.
After a discectomy, you can expect to feel pain at the incision site initially after surgery, as well as difficulty sitting or standing in one position for long periods. Non-dissolvable stitches or staples will be removed around five to 10 days after surgery, depending on the severity of your surgery. Your physician may recommend that you start physical therapy a few weeks or months after surgery.
Dr. Hany Demian, an expert in minimally invasive/chronic/spine surgery and CEO of the BioSpine Institute in Florida, says preparing before surgery is a good way to aid in healing after a discectomy.
“Stay hydrated. I tell my patients to drink a lot of water daily leading up to the surgery. Discs are made up of 80 percent water, so staying hydrated is essential for a smooth surgery,” Dr. Demian says. He also advises that patients start or continue supplements and a healthy diet. Collagen supplements and food high in collagen are recommended prior to the surgery. Patients should also ask their doctor what medication and supplements need to be adjusted or stopped prior to surgery.
Other remedies
If your pain isn’t severe and you don’t want to take pain medication, there are some home remedies that you can use. Applying hot and cold packs can relieve pain and swelling. Start with a cold pack, and after a few days, switch to heat packs to give relief and comfort.
Your healthcare provider may also suggest avoiding too much bed rest. Staying in bed can lead to stiff joints and weak muscles that may complicate your recovery. Stay in a comfortable position for no more than 30 minutes, then go for a walk. Start with short walks of 10 minutes or less, then gradually increase to 30-40 minutes.
Be mindful when resuming daily activities, paying attention to what causes pain and avoiding those activities. Exercise caution when doing activities that put too much stress on your lower back. These activities include lifting, sitting, bending and twisting, and driving.
Alternative and complementary treatments
Other alternative and complementary methods of treating a herniated disc can provide some relief for back pain. These options include:
- Massages to help relax muscles and ease tension
- Ultrasound therapy, which uses sound waves that produce vibrations which generate heat and relax tissue
- Acupuncture, which can help ease chronic back and neck pain
- Ozone injections, which can help heal discs naturally by reducing oxidative stress and inflammation
- Acupressure, which is similar to acupuncture and uses fingers, hands, and elbows instead of needles to provide some relief
Herniated Disc Recovery Timeline
When you know the signs that your herniated disc is healing, you’re better able to track your recovery timeline.
Initial Phase: Acute Pain Management
During the first part of your recovery timeline, your pain will shift from being sharp and constant to more intermittent and manageable. This happens as the pressure on the affected nerves reduces. There is usually intense pain in the affected area, and some muscle spasms. Expect radiating pain down your leg if the herniation affects a nerve in your lower back. This will be accompanied by numbness or tingling in the affected area, and difficulty moving or bending.
Intermediate Phase: Progressive Rehabilitation
In this stage, you’ll experience gradual improvement in your symptoms. You should have decreased pain intensity and frequency, with reduced muscle spasms. You should also have less numbness and tingling and improved range of motion.
Advanced Phase: Strengthening and Maintenance
At this stage, your pain should have significantly improved, but you may have some pain after strenuous activity and some residual stiffness or tightness in the affected area. During this stage, focus on maintaining your progress and preventing future episodes. You should practice good posture and body mechanics while continuing regular physical therapy exercises. This will help maintain core strength and flexibility.
Next, you will notice improved strength, coordination, and function as you’re able to perform daily tasks with less difficulty. One significant milestone on the recovery timeline is your decreased need for pain medication. You will feel less pain and be able to move on to a more independent and sustainable recovery.
The end of the recovery timeline ushers in a return of improved sleep patterns, daytime functionability, improved mood, and increased energy levels.
Frequently Asked Questions (FAQs)
How can I maintain a healthy lifestyle during my recovery?
Low impact exercises like walking, swimming, cycling, and yoga can help strengthen muscles that support your spine. This reduces pressure on your spinal column and promotes flexibility. Make an effort to get enough sleep so that your body can heal, and maintain a healthy diet.
Are there any specific dietary recommendations that can support my recovery?
Eat foods rich in sulfur, such as onions, leeks, garlic, and cruciferous vegetables (broccoli, cabbage, cauliflower, and brussel sprouts). It is important to drink enough water to maintain the health of your spinal discs. Avoid processed and fried foods, sugary foods, and beverages
How often should I follow up with my healthcare provider during my recovery?
You should follow-up regularly to ensure your healing is progressing well. The follow-up visits may include imaging and consultations about physical therapy. Your physician will determine how often you should follow-up with them.
Are there any ergonomic adjustments I should make at work or home to support my recovery?
At work, you can adjust your chair’s height so that your feet are flat on the floor and your knees are at a 90 degree angle. A chair that supports your lumbar region is also good. If you use a computer, make sure the monitor is at eye level. While sleeping, use a pillow under your back or between your legs to maintain neutral spine alignment.
Are there any new treatments or research developments for herniated discs?
Researchers at the University of Pennsylvania and the Corporal Michael J. Crescenz Department of Veterans Affairs Medical Center are developing a new biologic patch that could fix herniated discs in the back.3 The patch is activated by the body’s motion and plugs holes in the spine similar to a car tire.
A similar treatment is the two-step technique led by Lawerence Bonassar at Cornell University.4 It uses hyaluronic acid gel to replace leaked material and collagen gel to seal the hole. Regenerative medicine techniques have also been developed to treat disc degeneration.
Supporting Your Recovery
Diet, Exercise, and Lifestyle Changes for Herniated Disc Recovery
If you’ve suffered from a herniated disc, review your lifestyle to prevent a recurrence and hasten healing and recovery.
“Smoking avoidance is probably the best advice I can give,” says Dr. Brusovanik. Smoking can make you more prone to coughing, which can put pressure on your discs and strains your overall spine. This pressure can cause your spinal structures to weaken and increase your risk of further degenerative disc disease.
Pain Management Strategies for Herniated Discs
Functioning within the limitations of your pain is also important because painful physical therapy may make things worse. “Narcotics do not work for nerve pain that’s caused by a herniated disc, so knowing the risks of dependence, it’s best to not even try to treat nerve pain pharmaceutically,” advises Dr. Brusovanik.
He went on to share that giving the disc time to heal time and steroid injections may make a big difference. According to the American Academy of Orthopedic Surgeons(AAOS), pain medications don’t heal a herniated disc, they only relieve pain while the disc heals. Physicians are cautious about which pain killers they prescribe. Opioids are prescribed with care to prevent dependence and addiction.
You should also pay attention to ergonomics and proper body mechanics. Maintaining correct body posture can help prevent a herniated disc. Consider using a back brace to help keep your back straight and erect. A neck collar may help if you have a cervical herniated disc.
Psychological Support for Herniated Disc Patients
It will be helpful to develop coping strategies for life after having a herniated disc. Pay attention to habits you may develop while learning to cope with the chronic pain associated with having a herniated disc. Some people get used to walking or bending a certain way to avoid the pain associated with the herniated disc. Don’t get stuck with these habits. Practice stretches learned at physical therapy while you’re at home to help prevent this from happening.
Treatments for herniated discs can take time, and living with pain can cause emotional distress and depression. Stress and anxiety may also occur, so developing healthy habits and building a support system will support you through the healing and recovery process.
Conclusion
Recovering from a herniated disc can be painful and inconvenient but does not have to be unbearable. Understanding what is happening to your body, what to expect, and where to get help makes all the difference. At Commons Clinic, you can find top-ranked orthopedic specialists that provide wellness-focused care, from a diagnosis to recovery.
Healing happens gradually over several stages and will feel different for each individual. Each stage of healing has its unique characteristics and challenges. You can usually track your healing progress by how much your pain is decreasing, improvement of muscle weakness, and your overall improvement in movement and flexibility.
It is a good idea to see a doctor if you suspect that you may have a herniated disc. This will ensure that you get an accurate diagnosis and the right care. Your treatment for a herniated disc can range from allowing the herniation to heal on its own, medication for pain, physical therapy and even surgery. You should also expect to modify your diet and lifestyle to prevent a recurrence.
Sources
- National Institute of Health, Back pain in the United States
https://www.ncbi.nlm.nih.gov/books/NBK586768/#:~:text=It%20is%20estimated%20that%20up,some%20point%20during%20their%20lifetimes.&text=At%20any%20given%20point%20in,and%2014%25%20have%20neck%20pain, accessed August 20, 2024
- National Institute of Health,The Effect of Smoking on Spinal Fusion
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5779238/, accessed August 20, 2024
Cleveland Clinic, Herniated disc (Slipped, Ruptured or Bulging disc), https://my.clevelandclinic.org/health/diseases/12768-herniated-disc, accessed August 20, 2024
Penn Medicine News, New ‘Patch’ Uses Natural Body Motion to Fix Disc Herniation, https://www.pennmedicine.org/news/news-releases/2023/november/patch-uses-natural-body-motion-to-fix-disc-herniation, accessed August 20, 2024
Cornell Medicine, Two-step method patches herniated discs, https://news.cornell.edu/stories/2020/03/two-step-method-patches-herniated-discs, accessed August 20, 2024
National Institute of Health, Genetic background of degenerative disc disease in the lumbar spine, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6698496/, accessed September 3, 2024

About The Expert
Leonel Hunt, MD
Call
Leonel Hunt is a highly respected, board-certified orthopedic spine surgeon who focuses on the operative and non-operative treatment of pediatric and adult scoliosis, complex spine disorders, and artificial disk replacement using minimally invasive surgical techniques.
Learn more



 (310) 423-9834
(310) 423-9834