The Ultimate Guide To Artificial Disc Replacement Surgery
Artificial disc replacement surgery can offer relief, but what should you expect? Learn the procedure basics, recovery timeline, and potential benefits from top surgeons.
Artificial disc replacement surgery (ADR) is a promising surgical option for treating pain caused by disc degeneration in the cervical or lumbar spine. About 5.5 percent of the world’s population has symptomatic degenerative disc disease, so the need for effective treatment options is significant. 1 Prolonged neck or back pain can lead to missed work, poor sleep, and reduced overall activity. Thankfully, there have never been more options to treat back pain and restore function and mobility.
For certain patients, artificial disc replacement can reduce pain and improve your quality of life so you may return to your favorite activities sooner. In this article, we’ll outline the benefits of ADR surgery, requirements for surgical candidates, what the surgery entails, the expected recovery length, and other aspects of the procedure.
What is Artificial Disc Replacement surgery?
Artificial disc replacement (ADR) is a spinal surgery where a damaged or diseased disc of the cervical or lumbar spine is replaced with a prosthetic disc. During ADR surgery, the surgeon makes a small incision in the front of the neck or the abdomen to access the spinal column. Once the vertebra is exposed, the damaged disc is replaced with an implant.
Artificial discs vary in design and materials. The most common materials used are medical-grade metal alloys (such as titanium or cobalt-chromium), polyethylene (a durable plastic), or a medical grade thermoplastic with a zirconia-toughened alumina ceramic core.
Other names for artificial disc replacement surgery include:
- Total disc replacement (TDR)
- Cervical Arthroplasty
- Cervical disc replacement
- Lumbar disc replacement
- Lumbar arthroplasty
ADR is best for patients experiencing persistent back pain caused by a damaged disc that has not been effectively treated with other interventions, such as nonsteroidal anti-inflammatory drugs (NSAIDs, including ibuprofen and naproxen) or physical therapy. In addition to reducing pain, ADR also provides greater movement at the joint level for patients compared to spinal fusion, which is the most common surgical intervention for back pain.
What if I have a degenerative disc in my thoracic spine?
According to Sohrab Singh Virk, MD, a spinal surgeon at Northwell Health, artificial disc replacement is not typically recommended for treating back pain that originates in the middle area of the vertebral column, called the thoracic spine.
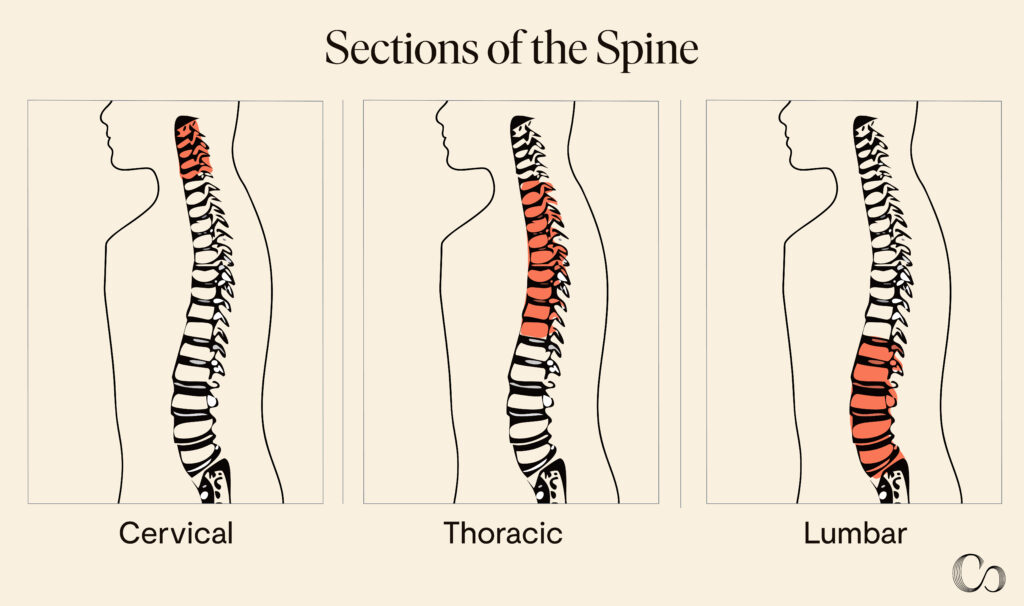
The 12 thoracic vertebrae do not require the level of mobility that the cervical and lumbar spinal regions do. As a result, thoracic spinal fusion (the alternative surgery) does not significantly reduce mobility at the joint level as it does in cervical and lumbar repairs, making it a more attractive option. The thoracic region also houses the ribs, sternum, lungs, and heart, which makes accessing the area during surgery more complex and risky.
For these reasons, no artificial discs have been designed for the thoracic spine. If surgery is needed to treat mid-back pain, the surgeon will likely choose a different treatment option, like spinal fusion.
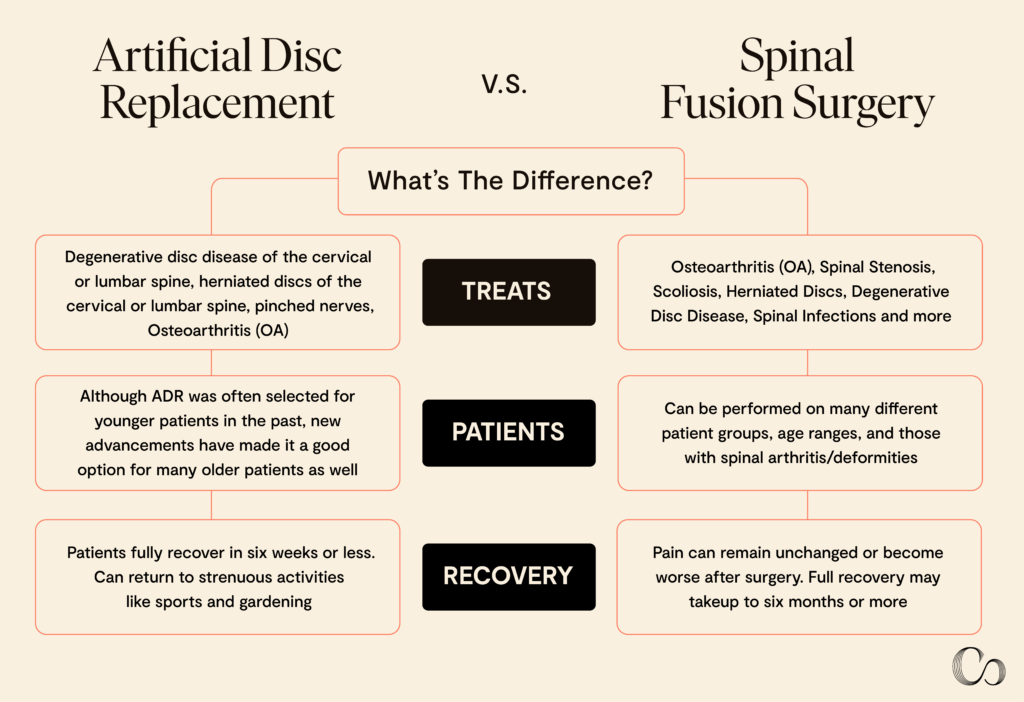
Artificial Disc Replacement vs. Spinal Fusion Surgery: What’s the Difference?
Both spinal fusion and artificial disc replacement are spinal surgeries that can treat back pain in the cervical and lumbar spine caused by degenerative disc disease. However, spinal fusion is often the default surgical option.
Spinal fusion, also known as disc fusion, treats numerous conditions, including osteoarthritis, spinal stenosis, spondylolisthesis, scoliosis, and herniated discs. During the procedure, two or more vertebrae are fused together using a bone graft, which reduces pain by eliminating unwanted spinal movement of the affected joint segment.
Spinal fusion treats:
- Osteoarthritis (OA)
- Spinal stenosis
- Spondylolisthesis
- Scoliosis
- Herniated discs
- Degenerative disc disease
- Spinal trauma
- Fractures
- Spinal infections
- Congenital spinal conditions
- Pinched nerves
Spinal fusion can be performed on many different patient groups and age ranges, including older adults and those with spinal arthritis or deformities. Moreover, because spinal fusion has been around longer, it is performed more often. Furthermore, fewer spinal surgeons currently receive training on artificial disc replacement.
In contrast, ADR surgery has stricter clinical requirements for patient selection.
Artificial disc replacement treats:
- Degenerative disc disease of the cervical or lumbar spine
- Herniated discs of the cervical or lumbar spine
- Pinched nerves
- Stenosis
- Osteoarthritis
ADR was traditionally selected for younger, healthier patients, but that is not always the case nowadays. According to Hyun Bae, MD, a trailblazer in the use of artificial disc replacement surgery for more than 20 years and a Commons Clinic physician, ADR has become a viable option for larger age ranges.
“Both young and older patients can benefit from disc replacement,” Dr. Bae says. “In fact, older patients may gain even more from it. While younger patients are already mobile and flexible, disc replacement helps maintain that flexibility, but the gain is modest. For older, stiffer patients, the impact of a disc replacement is far greater because it restores motion and flexibility.
And like many surgical procedures, the quality of the disc prostheses has significantly improved since their invention, so more surgeons are comfortable using them. Thanks to these technological developments and the growing body of evidence demonstrating positive outcomes for specific patients, ADR surgery has gained popularity since its introduction in the 1990s as an excellent alternative for treating back pain in select patients.2, 3
How do I know which surgery I need?
In terms of areas like flexibility, stability, and support for everyday activities like sports, artificial disc replacement surgery is a much more viable option compared to spinal fusion. According to Dr. Bae, spinal fusion decreases the flexibility of the spine. “Once you decrease the flexibility of the spine, that motion or that stress typically gets transferred to some other joint, usually in the spine itself, and that causes further problems down the line,” says Dr. Bae.
However, many surgeons recommend spinal fusion over disc replacement because they lack the training for the more specialized procedure of artificial disc replacement.
“The technique is difficult. It’s a highly specialized surgery. Most patients see surgeons who don’t specialize in artificial disc replacement (ADR). These surgeons either don’t know how to do it or were never trained in it—they were only trained in spinal fusion,” Dr. Bae adds. “So, when a surgeon tells you, ‘No, you can’t have a disc replacement; this needs to be fused,’ what they’re really saying is, ‘I don’t feel comfortable performing a disc replacement.’”
Many factors are considered when selecting which surgery is best for each patient, making it difficult to know which option is right for you. Your surgeon will review numerous factors to decide which surgical option is best. Their choice will also reflect factors like their medical training, clinical judgment gained from treating similar cases, and your spinal anatomy, among others.
Discuss all the available options with your surgeon. As a patient, you should always feel empowered to ask questions and share any reservations. Seek out a physician who is trained in both spinal fusion and artificial disc replacement to receive the best course of action. Many of Commons Clinic’s doctors have experience in and are highly knowledgeable about both.
No matter which option you choose, spinal surgery is a major decision, and you should feel comfortable and confident going into your procedure.
When Should You Get an Artificial Disc Replacement?
Because all surgeries come with risks, your surgeon may encourage you to try less invasive treatment options for your pain first. Many treatments are available for the numerous causes of back and neck pain. Some conservative treatment options include nonsteroidal anti-inflammatory medications (NSAIDs), physical therapy, steroidal injections, and massage therapy.
For patients who have attempted conservative pain management without success, surgical options may be considered.4 Your surgeon will perform a presurgical workup to thoroughly assess your condition. In addition to a thorough physical exam, medical history review, and detailed questioning, an ADR presurgical workup can include imaging such as:
- X-rays
- Magnetic resonance imaging (MRI) scans
- Computed tomography (CT) scans
- Discography
These imaging scans provide more information on the type of disc damage, where the damage is located, and details on your individual anatomy, all of which will help determine the type of disc implant the surgeon will choose.
When considering spinal surgery, it’s important to understand that spinal surgeons carefully consider which surgery is best for which patient. “Personal preference and surgical judgment play a significant role when choosing between ADR and fusion. There is a lot of gray area in the field of spinal surgery, and no one has all the answers,” Dr. Virk says.
Each surgeon’s experience and training are different and, therefore, they have different practice styles. Your surgeon will recommend the best course of action based on your anatomy, history, lifestyle, and preferences.
Additionally, your surgeon may want to perform one final step in your presurgical workup, called an epidural steroid injection (ESI). Steroidal injections are routinely given in joint spaces to reduce inflammation and pain. 5
In this case, injecting a steroid directly into the suspected joint space of your pain site can reassure the surgeon that it’s the correct vertebrae to replace. If the patient experiences pain relief from the injection, the surgeon knows they’ve located the right disc and can confidently replace it. If they don’t feel pain relief, additional testing is necessary before ADR surgery can be scheduled.
If you have a degenerative disc and you’re experiencing persistent pain in the back of the cervical or lumbar spine that has not resolved with conservative treatment, artificial disc replacement surgery might be an appropriate option to consider.
Questions to ask your physician
- Am I a good candidate for artificial disc replacement surgery?
- What type of artificial disc will be used, and why is it the best option for my condition?
- How will this surgery impact my mobility and flexibility compared to other treatment options?
- How experienced are you with performing artificial disc replacement surgeries?
- Can you provide patient testimonials or success stories from individuals who have undergone this procedure?
- What are the costs associated with the surgery, and does my insurance cover it?
- Can I see imaging or other diagnostic results that support the need for this surgery?
How Artificial Disc Replacement Surgery Works
Surgery will be scheduled after the surgeon completes their preoperative workup and reviews the test results, images, medical history, and assessment data. ADR is performed under general anesthesia, so the patient will be asleep the whole time.
The artificial disc implant
There are many types of artificial disc implants available to replace damaged discs: Each one offers its unique benefits, such as ease of insertion, elastic compliance, durability and MRI compatibility.
The surgeon carefully selects the best one based on the patient’s medical history, allergies, medical condition, and preference.
Anterior cervical discectomy procedure
The anterior cervical discectomy approach is used to access the vertebrae in both artificial disc replacement (ADR) and spinal fusion surgery. This approach involves making a small incision in the front of the neck. Through this incision, the surgeon carefully moves aside the tissues in front of the spinal column, including muscles, trachea, and esophagus to gain a clear view of the vertebrae.
In the case of ADR, once the vertebrae are visible, the surgeon proceeds to remove the damaged or degenerated disc. This step is crucial as it relieves pressure on the spinal cord and nerves, which may be causing pain, numbness, or weakness. The removal of the damaged disc creates space for the new artificial disc implant.
The artificial disc is then carefully placed into the disc space. These implants are designed to mimic the natural movement and function of a healthy disc, providing stability and maintaining the spine’s flexibility. Once the disc is in place, the surgeon uses X-ray imaging to confirm that the implant is positioned correctly and securely.
The entire procedure typically takes between two and three hours, depending on the complexity of the case, such as the specific part of the spine being operated on and the number of discs being replaced. During the surgery, surgeons take great care to minimize any disruption to the surrounding tissues and structures to ensure a smooth recovery process.
Benefits of artificial disc replacement surgery
Numerous studies have shown that ADR surgery can be as effective or more effective than spinal fusion in treating cervical and lumbar back pain caused by degenerative disc disease. This is especially true for single-level joint replacements. Patients who receive ADR also experience less pain in the first two years of recovery and often return to normal activities faster than those who undergo spinal fusion surgery. 6, 7
ADR also allows patients to maintain more vertebral mobility than spinal fusion, which is important in the cervical and lumbar spinal segments to maintain overall mobility and quality of life. Patients who undergo ADR surgery often report higher patient satisfaction and lower disability scores than those who have received spinal fusion. 8
For the small percentage of the 5.5 % of the world’s population that experiences back pain due to a degenerative disc disease and who do not respond to conservative treatments, ADR offers an effective treatment for their pain and the chance to significantly improve their quality of life. 1 2, 3
Risks and complications
As with any surgery, ADR carries certain risks. The most common risks include bleeding, infection, pain, a poor reaction to the anesthesia, blood clots, and poor wound healing. Risks and complications specific to ADR surgery are rare and mainly involve the implant itself. These include:
- Allergic reaction to the disc implant
- Temporary difficulty swallowing (called dysphagia)
- Implant failure or damage due to wear
- Improper implant size or fitting
- Implant migration
- Heterotopic ossification (HO)
Most of these implant-associated complications are less likely to occur with a highly experienced spinal surgeon who has performed many ADR surgeries.
A common complication after spinal fusion surgery is adjacent segment disease (ASD). 10 ASD typically requires another surgery and leads to another fusion if a fusion was performed initially. This can then cause a cycle of repeated ASD and repeat fusion surgery. Thankfully, ASD is rare in artificial disc replacement surgery and occurs in less than 3 percent of ADR patients. 11
How to minimize surgical risks and complications
To minimize surgical risks and complications in Artificial Disc Replacement (ADR) surgery, patients can take several proactive steps before and after the procedure. These include providing a comprehensive medical history, following pre-operative instructions, choosing an experienced surgeon, and adhering to post-operative care guidelines.
Comorbidities
To minimize the risk of a complication after surgery, there are steps the patient can take to limit those risks. Inform the surgeon and anesthesiologist of your medical history, allergies, and any adverse reactions you’ve had from anesthesia. Providing a comprehensive medical history reduces the chance that you will experience surgical complications and helps your care team provide you with the best possible experience.
Patients who smoke should stop smoking as far in advance of the surgery as they can, as smoking increases the risk of lung complications. Patients who have diabetes should carefully control their blood sugar before and after surgery to improve wound healing and reduce the risk of infection. Follow all medication instructions and take them consistently, especially antibiotics and pain medicines, in the postoperative period.
In addition to these standards, each patient will receive specific instructions based on their condition, age, fitness level, procedure, or comorbidities. Take down notes, or have a support person take notes, when your healthcare providers give you instructions to avoid missing crucial details.
If you have any questions or concerns about your procedure, write them beforehand and bring them to your appointment. It’s easy to feel overwhelmed when you’re receiving verbal instructions. By preparing questions in advance, you can ensure you won’t forget and that you feel confident going into your surgery.
Inactivity
After surgery, the surgeon will prescribe activity limitations. Try to be as active as possible while following your activity limitations, as movement will reduce the risk of blood clots and help you get back to your baseline faster.
For example, if your surgeon says you can walk during the first week after your operation, getting up and taking a lap around the house every few hours can help you recover faster and prevent complications such as developing blood clots in your legs, which can sometimes happen in the period after an operation.
Each patient will receive personalized instructions from the surgeon, so pay careful attention when they give them, ask questions, and then keep your instructions handy to reference in case you forget anything. Many patients like to keep them on their fridges with a magnet or jot them down in a notebook they keep close at hand.
In addition to these postoperative basics, the best way to avoid surgical complications from ADR surgery is to choose an experienced spinal surgeon. Many implant-related complications can be avoided when a surgeon has ample knowledge of the devices and how to measure and insert them correctly. In general, surgical complication rates decrease the more experienced the surgeon is, so spend time getting to know the surgeon and their experience level before scheduling surgery. 12
Questions to ask your spinal surgeon
- How long have you been in practice?
- How many of these surgeries do you perform each year?
- In your experience, how frequently do patients experience poor outcomes?
- What kinds of complications do you see most?
- How frequently do you have to perform additional surgeries on your ADR patients?
Both Georgiy Brusovanik, MD, an orthopedist and spine specialist at the Miami Back & Neck Specialists, and Dr. Virk recommend seeking a second opinion if you are unsure about the options presented to you. “Unfortunately, a large part of my practice is operating on patients who have had unsuccessful, sometimes unnecessary surgeries. This is your body, your life. I strongly recommend all patients get a second opinion before committing to spinal surgery.” Dr. Brusovanik says.
Dr. Virk agrees, “The single most important thing—more important than the type of spinal surgery or device—is that you feel comfortable and trust your doctor. If you’re unsure of anything, get a second opinion with someone who makes you feel comfortable and heard.”
Post-treatment
Immediately after surgery, patients are transferred to a recovery area, where their vital signs are carefully monitored while they wake up. Most patients are sent home the day of the surgery, but the surgeon may want them to stay overnight for additional monitoring.
Pain is usually the worst within the first 48 hours after surgery, so it’s essential to take pain medications on time and stay hydrated. For the first week or two, patients should not submerge their surgical site in a bath, pool, lake,or other body of water. However, they should keep the wound clean and change the dressing according to the directions they’ve received.
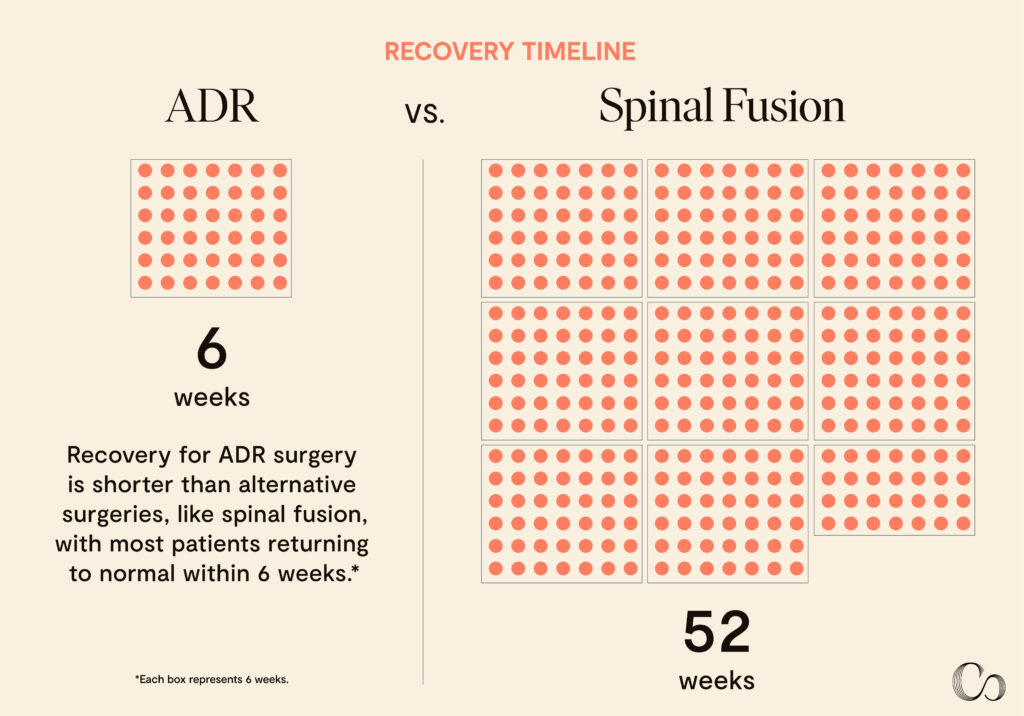
Recovery from ADR is much faster than spinal fusion surgery and typically takes two to six weeks. The surgeon may instruct the patient to wear a cervical collar during some activities, and the patient will be able to slowly return to activities of daily living during weeks two and three. The surgeon will likely schedule a follow-up visit in the first few weeks to check the incision site to assess proper healing and address any concerns.
Most studies on artificial disc replacements stop collecting data after 10 years, but many experts believe artificial discs can last for many decades, typically 40 to 70 years, without requiring a replacement. Discuss your surgeon’s experience with disc implant longevity. They are the experts on these types of implants and can give you details on the average experiences of all the patients they have treated.
How ADR Can Change Your Life
When you’re experiencing constant back or neck pain, your life is significantly impacted. From the activities you love, like sports, family time, and hobbies, to things that are easy to take for granted, like a peaceful night’s sleep, pain can rob you of the best parts of life.
Fortunately, for the right candidates, ADR surgery can significantly improve your quality of life and help you get back to moving pain-free relatively quickly.
“When you turn to look at somebody next to you, [when] you reach for an object, even as you breathe in and out, your spine is moving. And this motion is life, and we’re designed to move,” says Neil Bhamb, M.D., Commons Clinic orthopedic spine surgeon and director of concierge care. “The huge difference between fusion and disc replacement is motion. With disc replacement, you feel better right away, and a huge reason for that is that you’ve kept the physiologic motion that you’re never meant to lose with fusion.”
Effective Pain Treatment
Patients typically don’t consider spinal surgery unless they really need it, and they’re experiencing a level and frequency of pain that has completely disrupted their lives. For people who have symptomatic degenerative disc disease, ADR provides incredible pain relief. Patients frequently report high levels of satisfaction with their pain and quality of life after surgery.
More Spinal Mobility
ADR surgery maintains more regular movement of the spine, unlike spinal fusion surgery, which fuses vertebrae together and permanently reduces movement. ADR patients can return to strenuous activities like sports and gardening without pain and without compromising on freedom of spinal movement.
Faster Recovery
Unlike spinal fusion, ADR surgery is less invasive and does not require a bone graft, so recovery time is usually quicker. In just six weeks, most patients are able to return to work and light activity and report high feelings of satisfaction and little to no pain.
Frequently Asked Questions (FAQs)
How soon can I return to normal activities and work?
While each patient will have a unique experience, most patients recover sufficiently from ADR surgery in six weeks or less. During that period, you will likely have some limitations on physical activity to allow your body to heal and avoid unnecessary complications from over-exerting yourself.
Your recovery time will depend on many factors, especially the level of function you’re trying to reach. For example, most patients can return to a desk job in a week or two, while manual laborers and athletes may need up to three months to return to rigorous exercise.
Will I need physical therapy or rehabilitation post-surgery?
Physical therapy is often recommended after an artificial disc replacement to help improve mobility and flexibility and build back strength. Therapy often begins two weeks after a cervical disc replacement and at least four weeks after a lumbar disc replacement.
What signs of complications should I watch for after surgery?
The most common complications after any surgery are bleeding and infection. Your surgeon will provide detailed instructions on what to expect post-operatively and provide wound care instructions for your incision site. If you notice bleeding at the incision site, swelling, redness, increased pain, fever, or unexpected drainage during your recovery, contact your surgeon immediately.
Luckily, it is extremely uncommon for an artificial disc to have a mechanical failure. Most problems with ADR are due to placement. In these cases, they can be repositioned or changed to another artificial disc. As a last resort, the artificial disc replacement can be removed and the segment treated with a spinal fusion.
Key Takeaways
Artificial disc replacement is an effective surgical procedure that treats back pain in the cervical or lumbar spine caused by degenerative disc disease. Because it involves replacing the damaged disc instead of fusing it to another, as is done with spinal fusion, more mobility is maintained in the spine. By preserving spinal mobility, patients are able to resume activities they enjoy and return to an active, fulfilling lifestyle.
In addition to better spinal mobility, many ADR patients also experience shorter recovery times compared to spinal fusion, reduced pain during healing, and higher satisfaction scores. ADR surgery is one of the best interventions available to treat back and neck pain for patients with degenerative disc disease, and the sky’s the limit for the future of this surgery to help the patients who need relief the most.
Sources
Ravindra VM, Senglaub SS, Rattani A, et al. Degenerative Lumbar Spine Disease: Estimating Global Incidence and Worldwide Volume. Global Spine Journal. 2018;8(8):784-794. doi:https://doi.org/10.1177/2192568218770769
Davison MA, Lilly DT, Moreno J, Bagley C, Adogwa O. A comparison of successful versus failed nonoperative treatment approaches in patients with degenerative conditions of the lumbar spine. Journal of Clinical Neuroscience. 2021;86:71-78. doi:https://doi.org/10.1016/j.jocn.2020.12.033
Donnally III CJ, Hanna A, Varacallo M. Lumbar degenerative disk disease. PubMed. Published August 4, 2023. https://www.ncbi.nlm.nih.gov/books/NBK448134/
Lee YC, Zotti MGT, Osti OL. Operative Management of Lumbar Degenerative Disc Disease. Asian Spine Journal. 2016;10(4):801. doi:https://doi.org/10.4184/asj.2016.10.4.801
Patel K, Chopra P, Upadhyayula S. Epidural Steroid Injections. PubMed. Published 2021. https://www.ncbi.nlm.nih.gov/books/NBK470189/
Bai D, Liang L, Zhang B, et al. Total disc replacement versus fusion for lumbar degenerative diseases – a meta-analysis of randomized controlled trials. Medicine. 2019;98(29):e16460. doi:https://doi.org/10.1097/md.0000000000016460
Lang SAJ, Bohn T, Barleben L, Pumberger M, Roll S, Büttner-Janz K. Advanced meta-analyses comparing the three surgical techniques total disc replacement, anterior stand-alone fusion and circumferential fusion regarding pain, function, and complications up to 3 years to treat lumbar degenerative disc disease. European Spine Journal. Published online April 10, 2021. doi:https://doi.org/10.1007/s00586-021-06784-6
Yajun W, Yue Z, Xiuxin H, Cui C. A meta-analysis of artificial total disc replacement versus fusion for lumbar degenerative disc disease. www.ncbi.nlm.nih.gov. Published 2010. Accessed July 22, 2024. https://www.ncbi.nlm.nih.gov/books/NBK79792/
Sheng XQ, Wu TK, Liu H, Meng Y. Incidence of Heterotopic Ossification at 10 years After Cervical Disk Replacement. Spine (Philadelphia, Pa 1976)/Spine. 2023;48(13):E203-E215. doi:https://doi.org/10.1097/brs.0000000000004674
Birjandi A. Adjacent segment degeneration. Journal of Injury and Violence Research. 2012;4(3 Suppl 1):8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3571534/
Riew K, Schenk-Kisser J, Skelly A. Adjacent segment disease and C-ADR: promises fulfilled? Evidence-Based Spine-Care Journal. 2012;3(S 01):39-46. doi:https://doi.org/10.1055/s-0031-1298607
Lau, D., Deviren, V., & Ames, C. P. (2020). The impact of surgeon experience on perioperative complications and operative measures following Thoracolumbar 3-column osteotomy for adult spinal deformity: Overcoming the learning curve. Journal of Neurosurgery: Spine, 32(2), 207–220. https://doi.org/10.3171/2019.7.spine19656

About The Expert
Hyun Bae, MD
Call
Dr. Bae is a leading expert and pioneer in motion-preserving spine surgery. Known for avoiding unnecessary fusions, he specializes in artificial disc replacement.
Learn more




 (310) 437-7925
(310) 437-7925